Employee benefits consultant Taylor Lindsey sheds light on the paradigm shift of how employers are managing their employees’ health. In this episode, you’ll learn how employers can get a better ROI with their health plans, what changes in benefit offerings have come during the pandemic, and the need to be better incentivized to keep employees healthy.
Engage With Us
How to listen: shows.pippa.io/paradigm-shift-of-healthcare/howto
Archive of previous episodes: https://www.p3practicemarketing.com/paradigm-shift-of-healthcare/
Follow on Twitter: https://twitter.com/p3practicemktg
Full Transcript
Announcer: It’s time to think differently about healthcare, but how do we keep up? The days of yesterday’s medicine are long gone, and we’re left trying to figure out where to go from here. With all the talk about politics and technology, it can be easy to forget that healthcare is still all about humans. And many of those humans have unbelievable stories to tell. Here, we leave the policy debates to the other guys and focus instead on the people and ideas that are changing the way we address our health. It’s time to navigate the new landscape of healthcare together and hear some amazing stories along the way. Ready for a breath of fresh air? It’s time for your paradigm shift.
Michael: Welcome to the “Paradigm Shift of Healthcare” and thank you for listening. I’m Michael Roberts here today with my co-host, Jared Johnson. On today’s episode, we’re speaking with Taylor Lindsey, a partner at Employee Benefit Consultants, a benefit and HR firm. Welcome, Taylor. Thank you so much for making time to come on the show.
Taylor: Hey, guys. I really appreciate the opportunity and looking forward to the conversation.
Michael: Absolutely. We are too. We are too. So let’s jump right in. You know, what paradigm shifts are happening regarding the way that employers manage their employees’ health? In the midst of everything that’s going on, what are the changes that are happening?
Taylor: It makes me think about this I think actually in two different ways. But really, right now, what we’re seeing is a profound or pronounced focus on employee well-being, right? That employee as a whole. And I think that that means…to me, it means mental, physical, and financial well-being. And I think all three categories are certainly been put…the stress has been put on those three categories.
But the way you asked that question makes me think a little bit further. Right? So I think that employers have historically focused on how they manage the renewal process with health insurance, and how they manage or pick a health plan, quoting the same three or four insurance carriers every year, but it’s really not solving the problem. It’s really only addressing who’s purchasing that risk. And I think that the changes, back to the employee well-being, that are happening today, like, the employers are thinking about, you know, “What can we do as an employer to help our employee be better cared for, to increase access, to increase the quality of care?”
And at the end of the day, what we wanna do or the employer wants to do is to decrease cost. And I feel like that, you know, really nobody can do this alone. And it’s a complex system that’s been built kind of against the end consumer, and their employees need help navigating. I think employers are starting to wake up, they have woken up, and they’re continuing to realize that, you know, what they’ve been doing is not working and really what they’ve hoped for has not worked. And they’re really in a position to regain control and take back control and take this back into their own hands.
Michael: Yeah. You know, there’s so much that…as an employee that has to look at, like, what health plan that we have. And we have a nice health plan, and we have a nice insurance plan and everything, but there are still so many unknowns every step of the way. I’m going to get treatment. I have no idea how much it costs. We’ve had some various individuals that had the blessing of childbirth recently, but there’s no clear idea of like what it’s gonna cost going in. And there are so many uncertainties, even with good insurance and even with all that kind of information. So, you know, it’s interesting because the top of the show here, we’re talking about how your company is a benefits and HR firm. I guess, how is the human resources side of things being impacted in the midst of this? Because, you know, human resource is presumably more than just the insurance side of thing. How is that being impacted when you’re talking about the employee well-being? How is that aspect being affected?
Taylor: So the way we work is that we start to work with an employer to identify their goals, right? So what are their goals overall from a company and from a benefits perspective, HR and benefits perspective? And what we start to do is start to dive into what other categories can start to impact this program? Right? So HR, compliance, technology, well-being, you know, these other components, especially in the HR side. You know, we’re just seeing HR teams or either single people within an organization, depending on their size, they have been…they have earned their keep in the past four to six months, and really, it’s putting a stress on everyone. They’re having to deal with employee issues like they never dealt with from a complexity standpoint, but also to a number, right?
More of their employees are being impacted and fall into their category of being able to be their representative. Where that falls back into benefits is what can they do to help further support them? So, you know, I think from a bigger picture, everybody’s just strained. They’re certainly strained and having to redirect their focus where they never have before. And where we come into play is really trying to help them and allow them, give them the opportunity to be more strategic in their job versus reactive.
Jared: How much of that was starting to happen before the pandemic? Was there some momentum in this direction of feeling more responsibility towards managing your employees’ health, or is it almost…like do we attribute all of that to the pandemic or was it starting to happen? I don’t know which way it’s been. You know, I’m curious if it was starting to head that way.
Taylor: So I believe everything has kind of been…this category has been brewing for a long time, right? Healthcare and also in your HR side. It’s just given us an opportunity to accelerate it. You know, some in the good ways. We’re certainly trying to find the positives. And, you know, it’s got plenty of negatives associated to it. But it’s really just exacerbated the problems, right, in the healthcare system. It’s exposing all the cracks in our current system. Fee-for-service healthcare has caused way too many problems for everyone involved, and it’s completely taken the patient out of the center focus. Doctors have entered this business to treat patients to the best of their ability, and it’s…they’ve really lost that ability due to the amount of time that they have to spend with their patient.
So I think a lot of that has been exacerbated. I think from the HR side of the world, a lot of those problems have been because as the company grows and scales, you’re taking an office manager that’s growing into an HR category, or somebody who is historically HR is now managing a P&L item for healthcare. You know, it’s your number two or number three line item when in fact, you know…and that’s where…HR wasn’t really trained, or it’s not really the responsibility to manage benefits, it’s just where it falls most of the time, right? I see it as a relationship between CFO from the financial aspect of managing those dollars from a fiduciary responsibility to the HR side of doing what is in the best interest, and marrying that combination of friction and finance to do what is really the best possible investment we can give to our employees. Because at the end of the day, it’s their money, right? It’s an employee benefit. And I see the combination of those two working well together.
Jared: I definitely have some more questions for you around the financial aspects of it. I think there’s a ton there to definitely dive into. You mentioned that HR, you guys are helping to make HR more strategic. I’d love to hear if you can give us kind of an example that would, you know, be vague enough to protect everybody involved. But how…you know, so many times you do think of HR just being the response to an employee complaint or, you know, to whatever is going on in the office. How do you guys help be more strategic?
Taylor: So most of where we fall, we’re not so much in the day-to-day working hands-on with those employees, but what we’re doing is supporting that HR department in as much of an administrative responsibility as we can take on. We consult with employers to be able to handle all of their compliance obligations, to be able to support them with the tools and the resources that they need to be able to have more confidence in their job from a day-to-day perspective, right? So think about an office manager that’s grown, or the company has grown, and they’ve been put in this HR position. Well, if they don’t have the resources of being able to…they’re out googling these questions.
And that may take them half a day to find an answer, and they’re still not really sure if that answer is right. So, you know, we look at it and say, you know, “What are you doing today? What would this look like in an ideal world?” And then we work together to put together some resources, tools, and some accountability and an execution that helps them, you know, free up their days to be as high level and as available as they can be for those employees.
Michael: That’s awesome. So let’s get back to the finance side. So, you know, you’ve recently said that as businesses are struggling through this current economic downturn, the health plan is an easy place to find some extra money and that there’s money squandered in the way that health plans are being executed right now. So what is it that an employer should be thinking about to get a better return on investment with their health plan?
Taylor: Yeah. So, number one, I mean, I mentioned employers have fiduciary responsibility. So, with that being known and understood, personally, I believe that it starts with somebody that you can trust, right? So the transparent and properly aligned advisor. That’s at the head ground because employers don’t have time to do this nor is it really their role or responsibility if they can find an outside party that can help support them. So start with a transparent and properly aligned advisor, and allow yourself to be challenged, right? Think differently, challenge yourself, challenge your current partners, question them, try to find answers, and be curious.
But how I think about this a little differently is, you know, the money is there. We’re spending it already. It’s already a number two, number three line item. So where can we find this money? What are you currently spending it on? What can you do to better manage those dollars, and why are we chasing this money? Right? What are you gonna do with this money at the end of the day when we find it? That’s where we start to go into the how. Ten percent of the population spends about 80% of our claims.
That’s low-hanging fruit. Those are our outlier patients. And what we wanna do, is where we come in, is focus on the specialty situations in outlier patients. We start to find that money and reinvest it into the health plan. Right? We also may work with pharmacy partners, whether it be a local pharmacist or a transparent and properly aligned pharmacy benefit manager.
The way we think about this is, you know, holistically as a company, if we found this money, what are you gonna do to make your workplace better for your employees? And that’s where we start to get into a couple of core components, you know, value-based primary care, DPC. You had Dr. Johnson on here a couple of weeks ago. Again, taking the patient-focused back to the center and properly aligning, finding your community partners that are in a position to help solve your problems, and you’re also in a position to help solve theirs.
Michael: So my family, you know, we have a chronic patient in my family. And it’s something where we’ve had to do a lot to, you know, figure out how to make that work. The first time that we had this family member have to get a test, that, you know, we just were not expecting in any way. And the hospital told us, I think it was a Thursday, and they said, “Yeah, on Monday, when you come, we’ll need you to bring $2,000 for the payment.” And we’re like, “Yeah, that’s not just extra spending money that we have lying around for these kinds of things.”
And so it’s something where, you know, we’ve been able to figure out how to make that work. But, you know, I’m curious, so like for a family like ours, I know that our family is one that, you know, is definitely kind of on that higher end. So, like, can you talk through some of the specifics of how that would work out in terms of like, we have a chronic patient, so how does the health plan…how do we reorganize that to make that better for everybody?
Taylor: You know, I work in this system every day. And as a consumer of healthcare, it’s still a system that’s not easy to navigate. And so, number one, I think it’s our obligation, and part of our responsibility is to educate people on how the system works, and that this is one of the only…maybe the only place where there’s inverse…there’s misaligned incentives, number one, but also there’s inverse correlation to cost and quality.
As another colleague of mine mentioned, Carl Schuessler, you just have to understand or have the help and support to help you navigate the system in the most efficient way. And so, you know, we like to be able to arm our health plans with a concierge or advocacy services in which there’s individuals who are acting on the best interest of the employee and getting them to the right care. And in many times, you know, you have a direct primary care, value-based primary care doctor that can help them be that sherpa to understand, “Why are we getting this treatment? What happens if I get the treatment? What happens if I don’t get the treatment? How much is this going to cost?” So we start to just understand some basics and help arm those employees in this instance with the information to make better healthcare decisions.
Michael: That’s awesome. That’s super helpful. We’ve had the opportunity to have a few different patient advocates on, and the more that I hear about the role, whatever form that takes, whether it is a concierge or whether it’s your direct primary care doctor, having somebody guide you through that process seems so obvious but it’s so completely not how things are lined up right now. So I think that’s wonderful that you guys are building that in.
Taylor: Well, we appreciate it. And we just feel like it’s…you know, it’s been a system that’s been around probably since the early ’80s and which we’ve all kind of grown to trust. And as time has gone on, we’re starting to question it because the results seem to not be in the favor of those end-users, which are the employees and the employer paying for it. And so we knew something had to change, and we thought about it. And even the people that live and breathe the system every day don’t understand it.
Michael: There’s been so many times within our family where we’ve just had these questions like, “Are we heading in the right way?” Like as far as we know, we think we’re heading in the right way with the treatment plan, with all that kind of stuff, but there are so few sources for us to go and verify that right way approach.
Taylor: Yeah. And I think that that’s interesting. You know, you mentioned you guys have a great health plan, you know, 99% of your doctors are in-network, but you don’t know the good from the bad. You know, and that’s one thing. And then what if the diagnosis is not correct, right? I can’t remember the exact statistic, but a majority of cancer patients are misdiagnosed. And, you know, if you can embed something into a health plan that gives you the expertise to say somebody in number one and they’re in that category of care can look over your doctor’s shoulder and say, “Yeah, hey, good job, you’re doing this right,” or, “Hey, maybe let’s look at this from a different angle,” a second opinion type of approach to give that employee or that member that confidence to know that, “Hey, this treatment that we’re about to undergo, I feel a lot better and I feel a lot more certain because I have not only one doctor who is my local choice here, but it’s also an expert in this field and who has seen this hundreds of thousands of times.”
Jared: So, Taylor, how can employers be better incentivized to keep their employees healthy? You’ve mentioned there’s some momentum now, there’s more discussion about it, but the more we’ve had guests on recently who’ve really opened my eyes to the fact of so many problems in the healthcare system have to do with misaligned incentives. Parties are not incentivized to do certain things that are in the best interest of others. And so they don’t do it. They only do it if they have to, if they’re required to, if they’re mandated. So what are some ideas there? How can employers actually be better incentivized to keep their employees healthy?
Taylor: Sure. I mean, how? Like, how could you not focus on this? I mean, I don’t mean that as a joke, but, you know, we start to think about it. And it’s part of this process of helping people understand. And that’s really where it gets down to, is we’ve unintentionally had these blinders on in which we’ve asked questions and never gotten answers. So we finally just stopped asking questions. And we realized that there’s a direct correlation between your health insurance premiums and your healthcare claims. So when you start to think about it that way, if you wanna lower your health insurance spend or lower that budget item, how can we lower our claims? And that’s really just an active management.
You know, as I mentioned earlier, we always start with the low-hanging fruit, find those dollars and reinvest them back into your company. But it could be reinvest back into your health plan, improve your deductibles, or cut them in half, or get rid of them, making access to care better. You know, I think, again, that the employers are starting to wake up and realize that they hold the bag, they have more influence than they believe or more that they’ve been made out to believe. And I look for these employers to start standing up and to working together and speaking out about their problems. And really, I think that the opportunity is finding that audience, hopefully, providers and physicians that are willing to partner with them to really create something special for their employees and the communities in which they operate.
Jared: So if I can push on this even further, because I hear what you’re saying here, I’m thinking about, you know, kind of the employer out there that doesn’t buy this at face value, that they don’t get it, they don’t get the math, and they’re gonna need somebody to come in and demonstrate to them what we mean by, “How could you not focus on this? Here are the incentives. Here’s how the cost lowers.” You mentioned the correlation between your premiums and claims, for instance, is that a number to focus on in the case of an employer like this who still just needs help understanding how this works and how it’s worth it to them to keep their employees healthy? Like what data would they focus on?
Taylor: Yeah, I mean, there’s some simplified data like medical loss ratios. And that’s really just an equation to say how much premium have I paid in and how much of that premium have I paid in? Has the insurance company, at this point, paid out? That’s typically in your fully insured models. And the same thing happens for a self-funded plan. It’s how much money have I set aside or how much have I budgeted for compared to what’s being paid out? And you start to understand that, hey, maybe I’m overpaying, or maybe it makes sense for me to consider some alternative funding, whether it be level funding, partially self-funded, or a model… And I think the reality of that is, is it all starts back to access to your data. In the fully insured world we can’t…typically can’t find those numbers to look for and to focus on. I think that that’s a great question. It begins to help people understand that, “I need to be asking more questions.” So when we don’t have the data, we don’t know where to focus our attention and our dollars.
Jared: There you go. That makes a lot of sense. So then if we kind of, you know, take this further, if in a best-case scenario say we do see more momentum, more employers, this trend continues, more employers are paying more attention and realizing the advantages of this. They start to see the math more clearly. If more employers took a serious look at their benefit plans and how to get more value out of them, what could that do? Like what could the end scenario be, you know, the best case? How could that help improve the overall health system in America?
Taylor: Oh, this is a really great question and I appreciate it. A couple of things. Number one, it really makes me think about, like, why I’m in this business, why I’ve continued to do and to fight this model that is much easier to stick on the easy button. But as Carl Schuessler mentioned a couple shows back, you know, we’re in a sick care model versus the healthcare model. And I think if we can work together, these employers come together, create a relationship to understand that, you know, it’s not just for my employees, it’s for the community at large.
Provider systems also have problems. And the employer’s in a position to solve those problems. They have problems with revenue cycles, but yet the employer’s got a $3,000, $4,000 or $5,000 deductible. So how can we start to create this dialogue and these relationships within our communities? How can we work together to really focus back on to the patient and the overall health of that patient from a mental, physical, and financial perspective to get back to the roots and let go of the things that were in the past or should be the past?
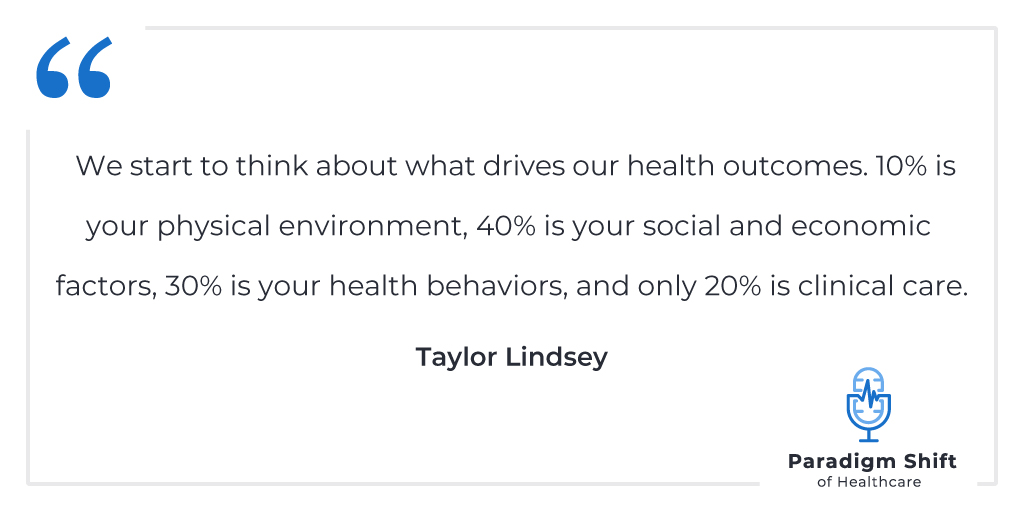
And, you know, I start to think about this from a bigger picture, why you’re competing against talent with local employers. Well, let’s step back a little further. And let’s step back and think about where we live and where we operate and what we do. We start to think about what drives our health outcomes. Ten percent is your physical environment, 40% is your social and economic factors, 30% is your health behaviors, and only 20% is clinical care.
So if we can work together better as a community, create healthcare being local, that means more dollars are staying in our local communities, which means then we can reinvest and make the places that we live more suitable to the lifestyles that we’re trying to live, more suitable for the diets that we’re trying to live, more financially healthier for our employees to have higher take-home pay and have less stresses. So I think from a bigger picture, there’s a lot that can be done for our local communities if we just look at our neighbors.
Jared: It sounds like that really is a tenet of how you work on plans, and advising and consulting is that local focus of how you can rewrite plans, and agreements, and contracts, and benefit packages to keep that money in a local community. I see a lot of advantages to that, and kind of starting to wrap my mind around this, but this is a really cool concept.
Taylor: Yeah, it’s taken a long time to understand but also to realize. You know, you can think about it from a lot of different angles. But it also made a lot more sense when I understood that the provider system also had problems, and that our clients were in a position to help them and vice versa. So when it is a win-win for both sides of the party, it just certainly puts everybody in a better position to what they’re doing today.
Michael: Can you go back and restate the percentages that you listed off just now? You said them so quickly and I was trying to write them down because I think that that’s such a great point that you were making. You were talking about how 20% of, you know, overall health kind of comes from care. What were the rest of those stats, sir?
Taylor: I think it’s 10% is your physical environment, 40% is your social and economic factors, 30% being health behaviors, and 20% is clinical care.
Michael: It’s fascinating because, you know, each one of the different factors there, depending on who you talk to gets so much overemphasis. You know, like, you talk to some healthcare providers and the 20% is the only thing that they really wanna talk about, and just on and on it goes. But it really is fascinating kind of how all that works together. But it really does make that impact of, hey, if we can change some of the social and economic in terms of like what’s available to the employee…what’s available to the employer after all this is kind of settled, that makes a huge difference. That’s awesome.
Taylor: Yeah, it really does. And, yeah, you start to think about it, I mean, how much you take home directly impacts what you eat, and what you eat directly impacts your health, and what…you know, it just starts this chain reaction to where we can get back to the root of the problem. And that’s why we’re…you know, as part of the Health Rosetta and the Health Rosetta Advisory, we’re really supportive of value-based primary care and, you know, getting back to that patient and provider relationship to help them have a more holistic view on who it is that they are treating.
Michael: And what size of company do you guys typically work with? I mean, what kind of companies should be thinking about these kinds of revaluations of their health plans?
Taylor: Certainly. I think our focus is in that 50 to 500 space. That is kind of our sweet spot.
Michael: Sure.
Taylor: But to scale this, quite honestly, sometimes it’s more difficult to do it on a smaller employer. You know, we have some partially self-funded or level-funded plans down into the 30s. Sometimes it’s more difficult than a larger employer because you have to manage the risk more carefully because one outlier can certainly disrupt a plan.
Michael: Yeah, that makes sense. We’ve had throughout the course of the show…one of the things that I’ve really wanted to focus on through all this, and we’ve had a chance to do this with a lot of different conversations, a lot of different guests, is how can people today make a difference in the healthcare system so that we’re not just waiting on legislation to do it for us, we’re not just hoping that somebody else will fix the problem? And really sounds like you’re really on this edge. Here’s a chance for employers to start making the difference. Here’s a chance for health plans to really start making the difference. So thank you so much for that. Thank you for sharing that information on the show. Because depending on how you feel politically, all those kinds of things, it’s either too much, or it’s not enough, or it’s whatever, but there’s so much that people can actually do in the now. And I love hearing those kinds of stories.
Taylor: We really appreciate the opportunity. Today, you know, from a patient end, even an employer perspective, I think the quickest, and the simplest, and easiest thing that they can do, ask questions. Be a 3-year-old and ask why over, and over, and over again because it’s the only way you’re gonna understand how it works. That’s the only way you’re gonna be able to move forward.
Michael: Absolutely. Absolutely. Taylor, thank you so much. Loved having you here. And everybody, I really hope you take that message to heart. Ask questions, first of all, and keep looking for those opportunities where each of us can start making the system better on our own. So thank you so much.
Taylor: I really appreciate the time and the opportunity.
Announcer: Thanks again for tuning in to the “Paradigm Shift of Healthcare.” This program is brought to you by P3 Inbound, marketing for ortho, spine, and neuro practices. Subscribe on iTunes, Google Play, or anywhere you listen to podcasts.
P3 Practice Marketing has helped orthopedic, spine, and neurosurgery practices market themselves online since 1998. Our focus is on helping practices expand their reach through increased patient recommendations and provider referrals.



